NERVE INJURIES
What are trigeminal nerve injuries and how are they caused?
The trigeminal nerve is the large sensory nerve that supplies feeling to your face, mouth, eyes, nose and scalp.
Nerve injury can sometimes result from dental treatments such as dental injections, root canals treatments, insertion of dental implants, removal of teeth, and other surgical treatments. These dental injuries affect the trigeminal nerve, usually involving the lower lip and/or tongue areas causing a mixture of pain, numbness and strange sensations that may be present all the time or intermittently.
Trigeminal nerve injuries can be extremely distressing. Although the majority of patients regain normal sensation and function within a few weeks or months, some are left with abnormal sensation or pain, which can cause major problems with speech and chewing as well as adversely affecting well-being.
Trigeminal nerve injury is the most problematic consequence of dental surgical procedures with major medical and legal implications; a significant number of complaints to the General Dental Council are related to dental implant treatment. The incidence of lingual nerve injury appears to have remained static in the UK over the last 30 years; However, the incidence of inferior alveolar nerve injury has increased: the latter being due to implant surgery and endodontic therapy.
Iatrogenic (caused by doctors or dentists) injuries to the third division of the trigeminal nerve remain a common and complex clinical problem. Altered sensation and pain in the orofacial region may interfere with speaking, eating, kissing, shaving, applying make-up, tooth brushing and drinking; in fact just about every social interaction that we take for granted. Usually after oral rehabilitation, the patient expects and experiences significant improvements, not only regarding jaw function, but also in relation to dental, facial, and even overall body image. Thus these injuries have a significant negative effect on the patient’s self-image and quality of life and the iatrogenesis of these injuries lead to significant psychological effects.
Signs and symptoms – What you may be experiencing
Trigeminal nerve injuries can cause episodes of intense, stabbing, electric shock-like pain and or constant burning/itching pain in the areas of the face where the branches of the trigeminal nerve are distributed: the lips, eyes, nose, scalp, forehead, upper jaw and lower jaw. Sometimes you may notice pain with touch or when a cold breeze hits your face.
Eating, speaking, drinking, brushing your teeth, shaving or applying makeup may all be difficult because of the changes in feelings and pain.
What are the risks of nerve injury in relation to dentistry?
Let’s start with a brief description of the main nerve – the trigeminal nerve – that can, very occasionally, be injured during dental surgery.
The trigeminal nerve is the largest peripheral sensory nerve in the human body and it is represented by an amazing 50% of the sensory cortex in the brain. The trigeminal nerve supplies the face, eyes, mouth and scalp with sensations such as touch, pain, and temperature.
It has three divisions, (hence the name trigeminal): these are called: the Ophthalmic division, the Maxillary division and the Mandibular division.
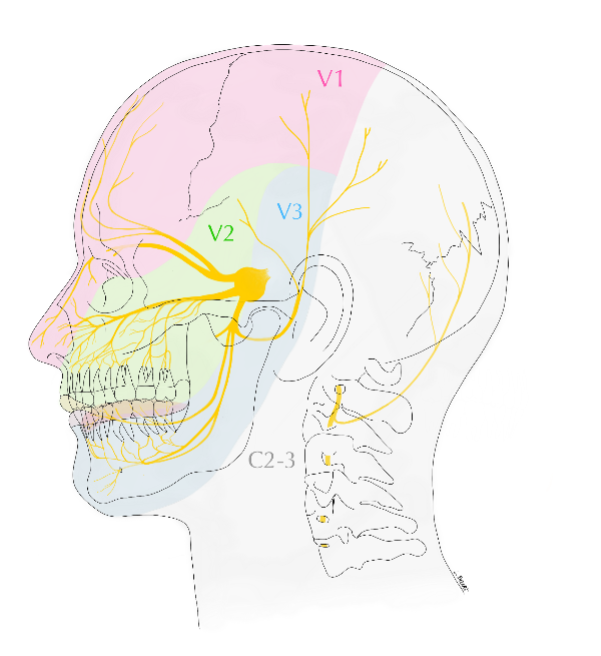
The trigeminal also gives nerve supply to make your chewing muscles work – the muscles of mastication.
What happens when a sensory nerve is injured?
Most nerve injuries related to surgery are temporary (less than 3 months). Some continued repair/regeneration can occur up to 18 months later, however if the initial injury is moderate to severe then it is less likely to get fully better, if at all.
After a nerve is injured during surgery, many patients at first feel numbness in the affected region and this may persist.
However, in some patients, instead of numbness, a troublesome sensation may develop which may become painful with certain stimulation. The patient may develop pain or discomfort which may be constant or intermittent. The pain may start spontaneously or started by moving, eating and touching. Bizarrely some patients feel numbness but get pain on touching the area or with temperature changes (cold or warm).
The types of changed sensation includes; shooting pains, burning, aching, stretching and pins and needles. Pain and discomfort can cause significant interference with daily function including eating, tasting, drinking, speaking, sleeping, kissing, shaving and in applying makeup normally.
Have you been injured?
If you have a nerve injury, you need URGENT assessment and possibly treatment as soon as possible in any case within 30 hours (go to the section Do you need urgent care on home page).
This is the case with root canal (‘endodontic’) and implant-related nerve injuries and some extraction related nerve injuries.
If you have had surgery or dental treatment and you notice any of the effects listed above after a local anaesthetic should have worn off, say 6 hours later, it is really important you seek advice from the surgeon, the hospital, or the dentist involved, or your GP if none of those can be reached.
It is often very difficult for the patient to come to terms with injuries caused by surgery especially if they have a major impact on their social and working life. Treatment of these injuries is very difficult and they are best treated if identified early on with referral to a specialist when necessary. Treatment usually involves counselling and reassurance, medication for pain and rarely surgery.
There are two main nerves that can be injured by dental treatment:
Inferior alveolar (lip and chin) nerve
Lingual (tongue) nerve
Both are sensory nerves (supply feeling) and do not move muscles (motor nerves)
Inferior alveolar (lip and chin) nerve injury
Outside the mouth the Inferior Alveolar Nerve, (a branch of the mandibular division of the trigeminal), supplies the skin over the whole side of chin, lower lip and vermillion border of the lip, (where the lip joins the cheek), on each side of the face.
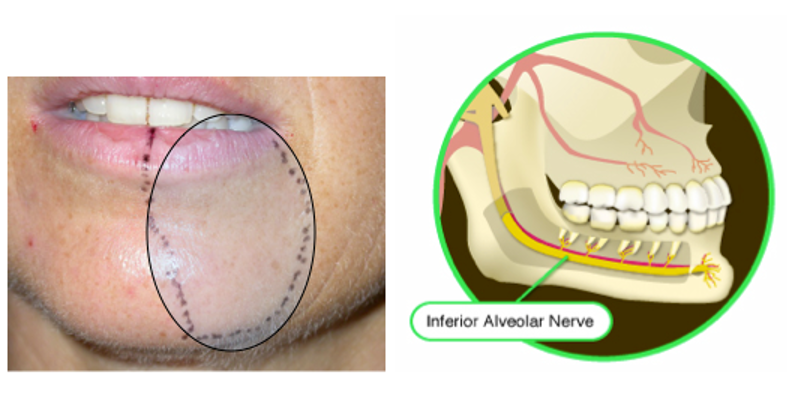
Sensory supply area of inferior alveolar nerve inside the mouth
On the inside of the mouth, the Inferior Alveolar Nerve (or ‘IAN’) supplies all the lower teeth, the cheek side of the gums and the skin on the inside of the lip.
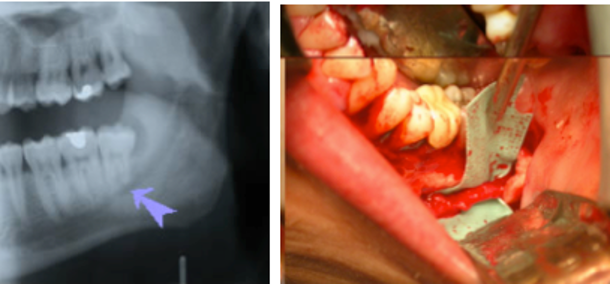
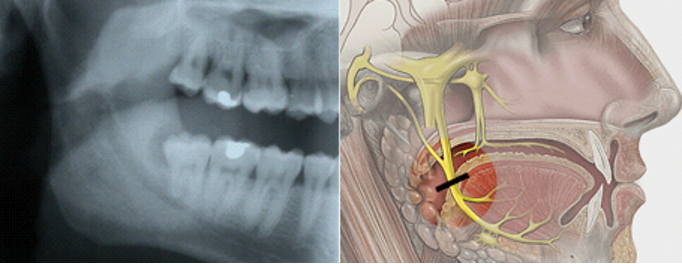
The Inferior Alveolar Nerve can be seen on the X-ray and photograph below. Notice in the photograph how it runs close to the lower wisdom tooth; this proximity is one reason why wisdom teeth can interfere with this nerve canal.
Causes of inferior alveolar nerve injury
Nerve injuries related to dental implant treatment is becoming an increasing problem. The incidence of implant related inferior alveolar nerve (IAN) nerve injuries varies from 0-40%. 25% of edentulous patients present with a degree of altered IAN function, thus reinforcing the guidelines on the necessity of preoperative neurosensory evaluation.
Some hints for you as the patient:
- Great care must be taken when selecting your clinician (avoid non specialists for complicated treatments and if you are in doubt contact the general dental council. We also suggest caution in seeking ‘cheap’ implant treatment abroad!).
- You should be advised regarding alternative treatments before you go ahead with implants
- You should have at least 2 visits including written and explicit consent that you should fully understand before signing
- You should be assessed using X-rays and sometimes special scans to see exactly where the nerve is and whether there is enough bone for the implant
- Scanning now available in many specialist practises and dental hospitals provides improved imaging for planning implant treatment with little radiation exposure. However, Cone beam CT evaluation can be less effective in identifying the IAN canal with poorer sensitivity and specificity compared with ‘pantomogram radiography’; (big Xray).
Third molar surgery
Wisdom teeth and some adjacent teeth have roots positioned very close to the lingual and inferior alveolar nerve canal in the jaw bone. Third molar and mandibular dental extraction related inferior alveolar nerve injury is reported to occur in up to 3.6 % of cases permanently and 8% of cases temporarily. Factors associated with IAN injury are age, difficulty of surgery and proximity to the IAN canal.
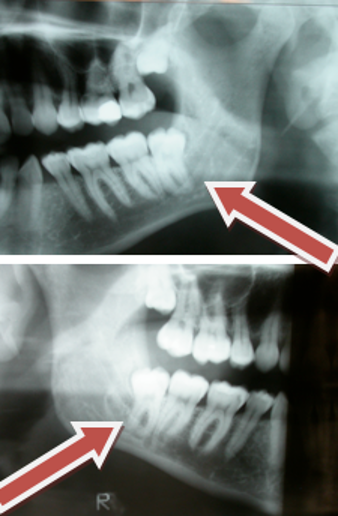
If the tooth is closely associated with the IAN canal radiographically i.e:
- superimposed on the IAN canal,
- darkening of roots,
- loss of lamina dura of canal,
- deviation of canal (Howe and Poynton 1969; Rood et al., 1983; 1986; Rud 1988)
then 20% of patients having these teeth removed are at risk of developing temporary IAN nerve injury and 1-4% are at risk of permanent injury (Howe and Poynton 1969; Rood et al., 1983; 1986; Rud 1988; Renton et al 2005).
The radiographs below illustrate 2 cases of ‘high risk’ mandibular third molars. In both cases the lower thord molar is crossing the IAN canal completely, there is darkening of the tooth roots and loss of lamina dura of the canal roof and floor.
Again caution is advised when selecting treatment. Oral surgery specialists, registered as such on the General Dental Council list, are best trained to carry out this work.
Therefore, the prevention of inferior alveolar nerve injuries in relation to third molar surgery is paramount and should ask: do you need the wisdom tooth removed?
Tara Renton chaired a group who have updated the Guidelines for Third Molar Surgery for the Royal College of Surgeons: Faculty of Dental Surgery. Parameters of care for patients undergoing mandibular third molar surgery. 2020. Available at: https://www.rcseng.ac.uk/dental-faculties/fds/publications-guidelines/clinical-guidelines/
A clinical decision that the tooth needs to be extracted should be based on NICE guidelines. Prophylactic surgery should only be undertaken when specifically indicated i.e. pre radiotherapy, pre chemotherapy or pre IV bisposphonates, none of which are included in NICE guidelines.
The clinician specialist must identify mandibular teeth at high risk of IAN injury based on plane radiographic features and/ or cone beam CT scanning. If deemed at high risk the patient must be made aware of the increased nerve injury incidence (increased risk 2% permanent and 20% temporary) and perhaps offered alternative procedures that may in course reduce the risk of injury.
- If the tooth is in close proximity to the IAN on plain film then;
- You should be warned of higher nerve injury risk (up to 10 times higher=20% temporary and 2% permanent compared with 2% temporary and 0.2% permanent form low risk wisdom teeth)
- You may be sent for Cone beam CT scanning which may further elucidate the relationship between IAN and tooth roots. If the tooth is non vital, or pathology associated with it, then tooth removal has to take place and the roots should be sectioned appropriately to minimise trauma to the adjacent IAN.
You may benefit by being offered a coronectomy procedure rather than removal of the tooth if appropriate (link to BDJ coronectomy paper)
The clinician should be aware that any mandibular tooth (lower 8,7,6,5 or 4) that if the tooth root is crossing the IAN canal, and displays the radiographic signs is associated with increased risk of IAN injury, there is increased possibility of damage to the IAN on removal of the tooth. The patient must be assessed accordingly, consented and treated similarly to high risk third molar teeth. The same assessment should be applied for these high-risk teeth as above.
Local anaesthetic injections (deep dental injections)
Injuries to inferior alveolar and lingual nerves are caused by local analgesia block injections and have an estimated injury incidence of between 1:26,762 to 1:800,000 inferior alveolar nerve blocks (Pogrel and Thamby, 2000; Haas and Lennon, 1995). More recently the incidence of nerve injury in relation to IDBs has been calculated as 1:609,000 but with a significant increase in injury rate with 4% agents (Gaffen & Haas 2009). These injuries are associated with a 34% incidence of neuropathic pain which is high when compared with other causes of peripheral nerve injury (Pogrel and Thamby, 2000). However, the true incidence is difficult to gauge without large population surveys. The problem with these injuries that the nerve will remain grossly intact and surgery is not appropriate as one cannot identify the injured region.
You may be at increased risk of nerve injury…
Based on present experience, you may be at increased risk of an injury, if:
- You experience pain on injection during treatment;
- You have multiple deep injections;
- The dentist uses a high concentration anaesthetic agent for deep injections.
Some practical hints for the patient considering treatment:
- Great care should be taken when selecting your clinician, avoid non specialists for complicated treatments and consider contacting the General Dental Council. Weigh up the risk factor if considering cheaper implant treatment abroad;
- Many clinicians are using a low-risk injection technique wherebye they give infiltrations, shallow injections next to the tooth. These replace deep ‘block’ injections. They use higher concentration anaesthetic in order to avoid unnecessary deep injections;
- If your clinician nevertheless recommends a deep injection, ask him if possible to avoid high concentration anaesthetic.
There isn’t much we can do with these nerve injuries aside from waiting for a recovery which may not always happen. But with these precautions your chances of an injury are likely to be reduced.
Dental implant related nerve injury
Dental implants require drilling a deep hole into the bone of your jaw in order to gain retention.
Occasionally the nerve canal is damaged during the preparation of the implant bed with resultant bleeding causing nerve damage. Unfortunately, if this happens these nerve injuries are painful and permanent unless the implant is removed within 30 hours of placement (see Do you need urgent care link). In addition, this nerve damage can occur on the anterior maxilla (upper jaw) related to dental implants.
Risk factors for these injuries include;
- Lack of appropriate planned safety zone with the Drill prep longer than implant depth causing damage to the inferior alveolar nerve canal
- Parasymphyseal region of the mandible where the premolar and first molar s are being replaced.
- Implant length over 8 mm
You may experience severe pain during drilling and or during the placement of the implant which indicates the surgery was too close to the nerve. After surgery when the local anaesthesia has worn off, you may notice that your lip feels numb and painful and the gum around the implant and adjacent teeth feels numb and painful. You need to seek urgent removal of the implant if you have numbness and pain after treatment.
Endodontics, or root canal treatment
Any tooth requiring endodontic therapy that is in close proximity to the IAN canal should have special attention given by the clinician. If the canal is ‘over prepared’ or the apex opened, chemical nerve injuries from irrigation of canal medicaments is possible. Endodontic nerve injuries are not be limited to those teeth close to the IAN canal in the jaw bone. In addition, this nerve damage can occur on the anterior maxilla (upper jaw).
The risk factors for endodontic inferior alveolar nerve injury include;
- Proximity of the tooth to the mandibular canal
- Over instrumentation
- Overfill
- Loss of apical seal during the cleaning of the root canal resulting in Chemical nerve injury (including; Calcium Hydroxide and Sodium hypochlorite)
You may experience severe pain during drilling and or during the root canal which indicates the surgery was too close to the nerve.
After surgery when the local anaesthesia has worn off, you may notice that your lip feels numb and painful and the gum around treated tooth and adjacent teeth feels numb and painful. You need to seek urgent removal of the implant if you have numbness and pain after treatment.
Lingual (tongue) nerve injury
What does this nerve supply sensation to?
The lingual nerve supplies sensation to each side of the tongue on the top and underside of the tongue. It also supplies the floor of the mouth and lingual gums of the lower teeth.

Where is it?
The lingual nerve doesn’t show up on xray as it isn’t in a bony canal. It runs very closely to the wisdom teeth in soft ling tissue running forward to supply feeling to the anterior 2 thirds of the tongue:
Causes of lingual nerve injury include:
Third molar surgery
The most common cause of Lingual Nerve Injuries is third molar (wisdom tooth) surgery, with a reported incidence of 1-20% temporary and 0-2% permanent (Mason 1988; Blackburn 1990; Renton & McGurk 2001; Renton & Yilmaz, 2011). 88% of lingual nerve injuries associated with third molar surgery resolve (Mason 1988; Blackburn 1990). Persistence of any peripheral sensory nerve injury depends on the severity of the injury, increased age of the patient and the time elapsed since the injury. There are specific guidelines by the Link to FDS RCS Third molar guideline paramaters of care regarding whether you need your wisdom tooth removed.
Local anaesthesia
Lingual nerve injuries can be caused by deep block injections at the dentists (similar to risks for spine injections and epidural injections.

